Psoriasis: causes, symptoms, diagnosis and treatment.
Psoriasis is a chronic non-communicable disease that can affect various organs: skin, joints, heart, kidneys.
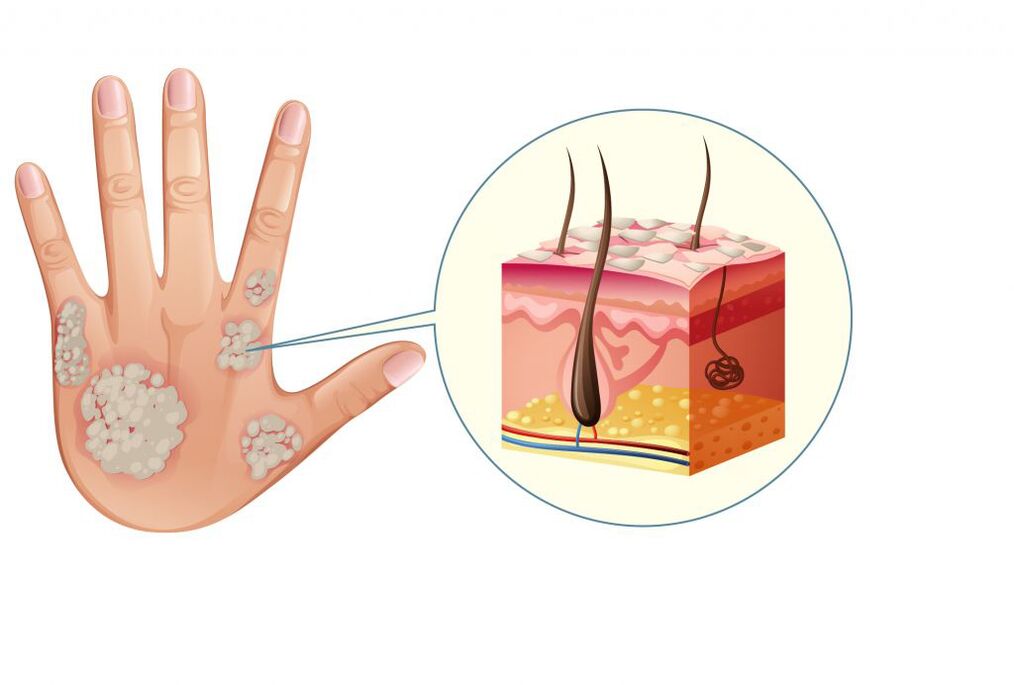
Most of the time, mild psoriasis appears on the skin as well-defined, pinkish-red papules (nodules that rise above the surface of the skin), which coalesce into silvery-white scaly plaques.
In moderate and severe forms of the disease, the inflammatory process causes damage to the musculoskeletal and cardiovascular systems. Psoriasis has a relapsing course (recurrence of symptoms after full or partial recovery) and a tendency to cause comorbidities that impair the quality of life of patients.
Causes of psoriasis
The disease can be based on various triggering factors. However, it is not yet known exactly which of them are primary and which are secondary. The dysfunction of the immune system is considered the main cause that explains the appearance of psoriasis. The cells intended to destroy the disease-causing agents begin to attack their own cells (primarily the skin). As a result, an inflammatory process develops, causing accelerated cell division of the epidermis (epidermal hyperplasia) and the formation of psoriatic papules and plaques.
An inadequate immune response is most often due to genetic characteristics.
Psoriasis is very often inherited.
Currently, more than 40 chromosomal regions have been identified that are associated with the risk of developing psoriasis. The onset of the disease can be caused by a weakening of the immune system against the background of stress, infectious and endocrine diseases. Psoriasis often accompanies allergic and immunodeficiency conditions, which are based on a violation of the immune response. Also, psoriasis can be triggered by certain medications (antidepressants, beta-blockers, non-steroidal anti-inflammatory drugs).
Psoriasis classification
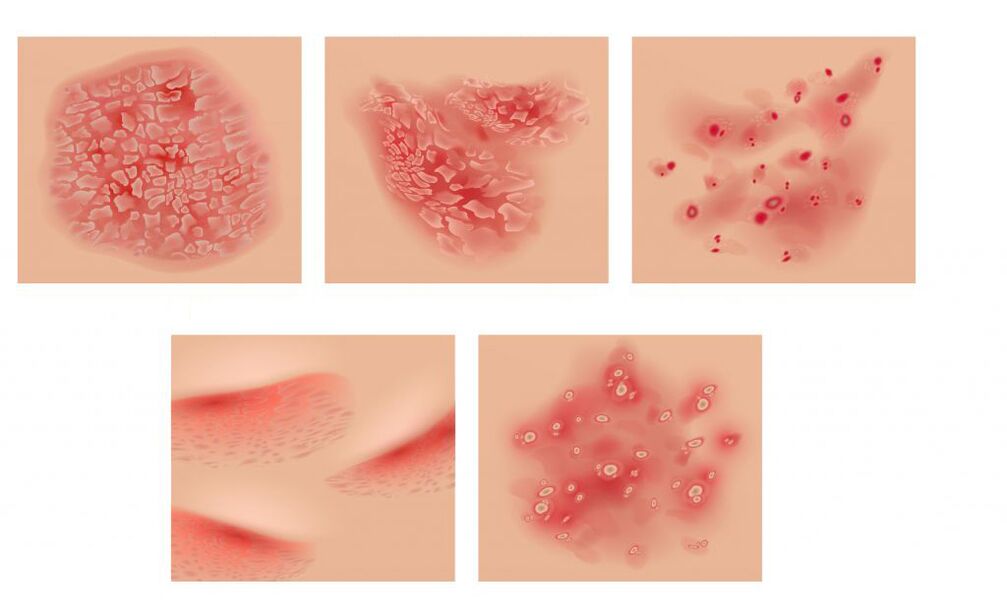
Depending on the localization of the pathological process, several types of psoriasis are distinguished. The most common is vulgar, orcommon psoriasiswhen well-defined pinkish papules appear on the skin, merging into plates covered with silvery-white scales. In case of damage to the scalp (seborrheic psoriasis) rashes in the form of yellowish scales can descend on the forehead, forming a seborrheic "crown". In patients with metabolic disorders, plaques may exhibit exudate, a fluid secreted during inflammatory processes (exudative psoriasis). In childhood and adolescence, especially after streptococcal infections, the disease can become acute, with many bright red, tear-shaped papules appearing on the skin with slight scaling and infiltration.guttate psoriasis). Sometimes there is pustular psoriasis, which is characterized by the appearance of pustules at the bottom of the reddened skin, most often on the arches of the feet or the palms of the hands.Psoriatic erythrodermacan occur against the background of exacerbation of ordinary psoriasis under the influence of provoking factors. Dry white scales cover the skin, which becomes bright red, swollen, and hot to the touch. run very hardGeneralized Zumbusch psoriasis. It is characterized by the appearance of small purulent vesicles on the reddened skin, which merge to form "purulent lakes".Psoriasic arthritisaccompanied by joint damage and develops simultaneously with rashes or precedes them.
psoriasis symptoms
The cutaneous form of psoriasis is accompanied by the appearance of bright pink dotted papules, sometimes in the form of droplets. Upon merging, they form plates covered with silvery-white scales.
Rashes are found on the extensor surfaces of the arms and knee joints, on the scalp, on the lower back and sacrum.
The upper layer of plaques is made up of scales of dead epidermis that are easily removed. Initially, they occupy the center of the plate, and then fill its entire area. When the scales are removed, a shiny bright red surface is revealed. Sometimes the plaque is surrounded by a pink border, an area of increased growth, while the surrounding skin is unchanged. The rash is accompanied by intense itching. With psoriatic erythroderma, patients develop fever (fever with chills) and severe itching against the background of rashes all over the skin and enlarged lymph nodes.
With a prolonged course of the disease, hair and nails may fall out.
Generalized Zumbusch psoriasis is very difficult. Purulent rashes cover the entire skin and are accompanied by severe fever and intoxication. Psoriatic joint damage is characterized by pain and reddening of the skin over the joint surfaces. Any movement is difficult, inflammation of the ligaments and tendons develops. With psoriasis, the nail plates are very often affected, while pinpoint depressions appear on the nail surface (a "thimble" symptom).
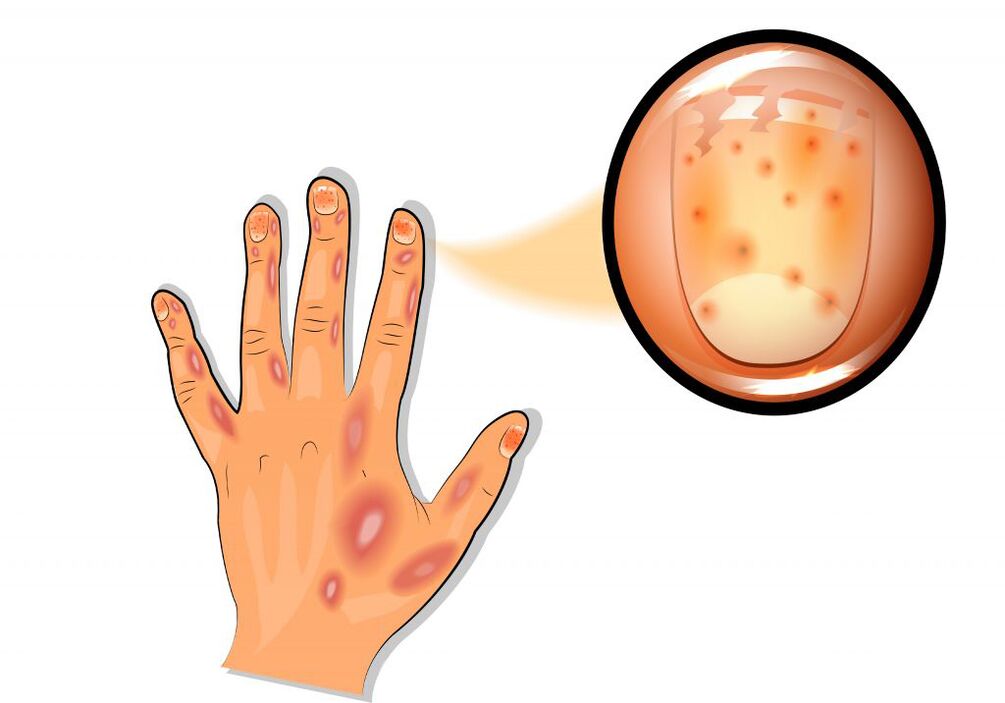
Small reddish and yellowish-brown spots appear under the nail plate at the base (symptom of "oil stain"). Dystrophic changes in the nails and hair often develop.
In children, especially infants, the symptoms of psoriasis have their own specificities.
In the area of redness that occurs in the skin folds, effusion and slight peeling of the upper layer of the epidermis may occur. This image resembles diaper rash or candidiasis. Sometimes rashes appear on the skin of the face or in the genital area.
Diagnosis of psoriasis
It is possible to identify the disease on the basis of the symptoms of the psoriatic triad (white stearic surface of the papule; shiny reddish film after peeling off the scales and pinpoint blood protrusion after their removal).
An additional feature is the Koebner phenomenon. It lies in the fact that in the area of skin irritation, after 7-12 days, erythematodesquamative rashes appear (areas of redness and peeling in the area of scratches, scratches). Sometimes, to confirm the diagnosis, histological examination of a biopsy of the affected skin area is performed. In addition, a clinical and laboratory examination is necessary: a clinical blood test, a biochemical blood test (total protein, protein fractions, C-reactive protein, ALT, AST, LDH, creatinine, electrolytes: potassium, sodium, chloride, calcium).
Which doctors to contact
If rashes appear, which often occur against the background of infectious diseases, skin injuries, stress, you should consult a therapist or dermatologist. In case of systemic damage to the patient's body, he may be referred to an ophthalmologist, endocrinologist, gynecologist or other specialists.
Treatment
Psoriasis affects both the skin and the musculoskeletal system, as well as the internal organs. When rashes appear only on the skin, local preparations of glucocorticosteroids, ointments containing synthetic analogues of vitamin D3, activated zinc, salicylic acid and other components are recommended. Hormonal creams should be used with caution on skin prone to atrophy.
It is necessary to take into account the possibility of hormonal disturbances with prolonged use of steroid creams.
The effectiveness of hormonal creams is increased in combination with salicylic acid, analogs of vitamin D. For the treatment of severe forms of psoriasis, aromatic retinoids of the second generation are used, which are based on acitretin. The drug slows down the proliferation of epidermal cells, normalizes the keratinization process and has an immunomodulatory effect. Phototherapy (medium wave UV therapy and PUVA) in combination with retinoids is also recommended. As systemic therapy, the doctor may prescribe immunosuppressive agents. If necessary, prescribe detoxification and desensitization therapy, plasmapheresis.
psoriasis complications
In 10% of patients, psoriatic arthritis develops, affecting the spine, joints of the arms and legs. Patients suffer from joint pain and morning stiffness. Features of psoriatic arthritis include asymmetry of the places of its manifestation, which can be combined with nail damage. Psoriasis is often accompanied by concomitant or comorbid diseases.
Due to inflammatory vascular lesions, the risk of coronary heart disease and stroke is increased.
It is also possible to develop diabetes and Crohn's disease. In some cases, complications of psoriasis can lead to disability.
Psoriasis Prevention
Measures to prevent psoriasis are primarily aimed at strengthening the immune system. Skin care should include hydration and nutrition. With a predisposition to allergies, it is necessary to monitor nutrition, avoiding fatty and spicy foods, excessive consumption of carbohydrates, potatoes. A mandatory component of psoriasis prevention should be vitamin therapy.
In addition, the functioning of the immune system depends to a large extent on the state of the nervous system. People who are hyper-responsible, have a busy work schedule, and experience constant negative psychoemotional impact are more prone to autoimmune diseases, including psoriasis. Therefore, the prevention of psoriasis, together with physical healing measures (abandonment of bad habits, physical activity), must also contemplate the achievement of psycho-emotional well-being.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For proper diagnosis and treatment, you should contact your doctor.























